Why Indiana and Mike Braun are getting national attention for its Medicaid crackdown
Camille Beeson on Medicaid waitlist affecting Indiana seniors, assisted living facilities
Camille Beeson, regional director of operations at the Wyndmoor of Castleton, speaks on how Indiana’s waitlist for Medicaid waiver services is affecting seniors and assisted living facilities.
As Minnesota’s Medicaid program broils in the hot seat over a recent round of federal fraud indictments, Indiana’s Medicaid program is gaining national attention as a counter-example for its efforts to crack down on program eligibility and waste.
Indiana’s Medicaid policies certainly have their critics, though, as some Medicaid recipients linger on waitlists for care and the state has made it more challenging for Hoosiers to stay on Medicaid.
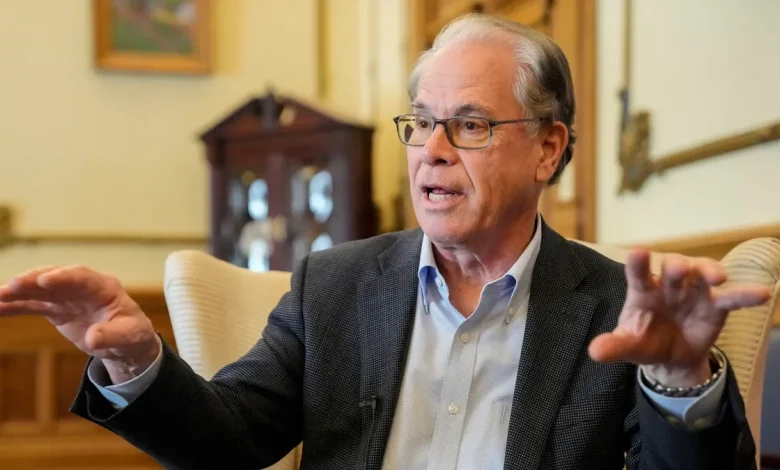
The Wall Street Journal’s editorial board named the comparison a “tale of two Medicaid states,” and Gov. Mike Braun, whose administration ushered in a number of changes this year to try to reduce enrollment, appeared on Fox News on Dec. 27 to talk about it.
“We’re just picking that low hanging fruit,” he said, “and that’s why we’re going to lead the country.”
Federal prosecutors recently accused six more people of defrauding Minnesota’s Medicaid programs, capping a growing list of indictments costing the state hundreds of millions of dollars. The various alleged schemes, beginning with a child nutrition program in charges filed three years ago, roughly involve nonprofit or business owners filing inflated or fraudulent claims to state Medicaid in order to allegedly turn a profit.
Democratic Gov. Tim Walz has taken flak from national Republicans for these indictments. The House Oversight Committee this month launched an investigation into suspected fraud in a number of Minnesota programs. Walz has applauded the federal charges and launched a new fraud detection program in his state.
But the Wall Street Journal lifted Indiana’s program as an antidote, citing a recent Medicaid forecast that shows the state is expected to spend about half a billion dollars less than it previously anticipated over the next two years.
Indiana’s new lower projection is chiefly due to a decrease in Medicaid enrollment by about 10% from January when Braun took office to October of this year.
Through a combination of executive orders and a new state law passed in April, the Family and Social Services Administration has ramped up the frequency of eligibility checks by cross referencing databases from both state and federal agencies, from income and employment records to the death registry. State agencies are also no longer allowed to advertise Medicaid programs or benefits.
In his Fox interview, Braun mentioned a few examples of “low-hanging fruit” the state found, including people who should have been on Medicare instead of Medicaid, and people who were “double-dipping.”
In sharing the new Medicaid forecast earlier in December, FSSA Secretary Mitch Roob attributed the enrollment drop chiefly to the halting of advertising, as well as a policy change that requires enrollees to respond to a mailer as part of the Medicaid redetermination process, or else be dropped. Previously, it was optional to respond.
He said he is uncertain about how long the enrollment drops will last, and cautioned that Indiana is not in the clear in terms of managing Medicaid growth.
“We have not made Medicaid boring yet,” Roob said. “This is not the beginning of the end, it’s the end of the beginning for rebalancing the Medicaid program.”
State spending on Medicaid is projected to grow by 3.2% in 2026, compared to a previously estimated 9.5%. The growth is expected to continue into 2029, when state spending could top $5.3 billion.
Indiana found itself in a similar situation to many states, including Minnesota, whose spending surged after the pandemic. In 2019, Indiana spent $2.2 billion on Medicaid, compared to $4.4 billion in 2025.
A huge and unexpected jump occurred between 2023 and 2024, when budget writers discovered a $1 billion budget shortfall due in part to explosive growth in certain programs. FSSA responded in part by implementing waitlists for waiver programs, like assisted living facilities, and Roob said he sees no end in sight for those.
The picture is further complicated by the fact that the rates providers charge are anticipated to rise significantly in 2026. Roob said he believes that’s because more often than not, healthier people have left the Medicaid rolls, and sicker patients have remained, making the risk pool higher.
The Wall Street Journal also noted the further reforms Indiana is considering, including a series of oversight measures suggested for the state’s autism behavioral therapy program in light of unsustainable growth and a federal audit finding tens of millions in “improper” payments.
If Republicans in Congress “want to show voters that it’s worth re-electing a Republican majority next year, they could follow the Hoosier reform example,” the editorial board wrote.
Contact IndyStar Statehouse reporter Kayla Dwyer at [email protected] or follow her on X, formerly Twitter, @kayla_dwyer17.




