FDA approves first new antibiotics to treat gonorrhea in decades, with hope to combat drug resistance
For the first time in decades, the US Food and Drug Administration has signed off on new antibiotics to fight gonorrhea. The approvals come at a critical moment: The sexually transmitted infection is growing harder to treat, and cases continue to climb nationwide.
The FDA announced Friday that it has approved zoliflodacin, sold under the name Nuzolvence, as a single-dose oral treatment for gonorrhea in the urogenital area in adults and adolescents 12 and older who weigh at least 77 pounds. The medication is administered as granules that dissolve in water. The nonprofit Global Antibiotic Research and Development Partnership collaborated with Innoviva Specialty Therapeutics Inc. to develop the drug.
And GSK announced Thursday that the FDA had approved its medication gepotidacin, with the brand name Blujepa, as oral tablets to treat urogenital gonorrhea in people, 12 and older who weigh at least 99 pounds, who have limited or no alternative options. In March, the drug also was approved to treat urinary tract infections in women.
“These approvals mark a significant milestone for treatment options for patients with uncomplicated urogenital gonorrhea,” Dr. Adam Sherwat, director of the Office of Infectious Diseases in the FDA’s Center for Drug Evaluation and Research, said in a news release Friday.
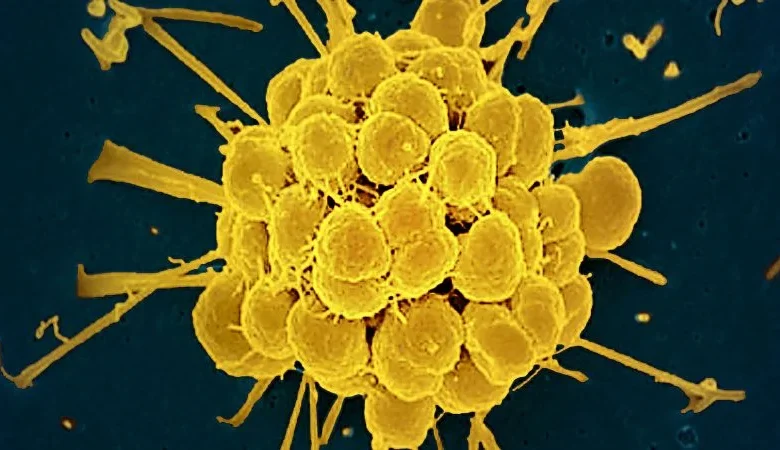
Effective treatment options for gonorrhea have been shrinking fast in recent years. The bacteria responsible for the infection, Neisseria gonorrhoeae, has developed resistance to many of the medications widely used to treat it, rendering many previously used first-line antibiotics virtually useless.
“We’re proud to have delivered the first new class of antibiotics for gonorrhoea in over three decades and a new oral option for US patients. The ability of N. gonorrhoeae to develop resistance to currently available options, including standard of care, makes it important to expand the range of effective oral treatments,” Dr. Tony Wood, GSK’s chief scientific officer, said in a news release.
The current standard of care includes an injection of the antibiotic ceftriaxone, which means patients need to go into a clinic or doctor’s office for treatment.
But both of the newly approved medicines are taken by mouth. No needles or clinic visit may be required, which could make treating gonorrhea much more convenient, said Dr. Manica Balasegaram, executive director of the Global Antibiotic Research and Development Partnership.
Additionally, “zoliflodacin is a single-dose treatment, which also gives it a big advantage. This means that you can administer this treatment in different health care settings, but you don’t need to have all the facilities to inject an injectable,” Balasegaram said.
“When you’re dealing with emerging drug resistance, then you have to look at different options. And this is why it’s really important to bring these new treatment options onto the table, specifically when they can be easier to administer, and that’s very important from a public health perspective in trying to control a disease like gonorrhea,” he said. “These are urgently needed drugs for a disease that is becoming out of control and becoming much more difficult to treat.”
The need for easier, more accessible treatment is especially pressing in the US. Gonorrhea and other sexually transmitted infections, or STIs, have become more common, with reported cases of three infections – chlamydia, gonorrhea and syphilis – jumping 90% in 2023 compared with about two decades prior in 2004, according to data released last year by the US Centers for Disease Control and Prevention. In 2023 alone, more than 2.4 million cases of STIs were reported.
Without treatment, gonorrhea can lead to major health problems. In rare instances, it can even spread to the bloodstream or joints. Among women, untreated gonorrhea can cause an infection of the reproductive organs called pelvic inflammatory disease, raising the risk of pregnancy complications and infertility. In rare cases among men, gonorrhea also can lead to infertility as a long-term consequence. There is no licensed vaccine to prevent gonorrhea infections.
Adding to the challenge, the infection is becoming increasingly difficult to treat. The bacteria continues to outsmart many of the antibiotics that doctors have long relied on, meaning those drugs are no longer as effective at treating the infection.
In some cases, bacteria can develop antimicrobial resistance because antibiotics may be overused unnecessarily or misused when people don’t finish their course of treatment. As a result, the harmful bacteria can still survive and because of the overuse or misuse of treatment, they may have become familiar with the medication, adapting to it and possibly becoming resistant to it.
As a new drug, zoliflodacin was developed to remain active against resistant trains of Neisseria gonorrhea that no longer respond to commonly used drugs like ciprofloxacin, ceftriaxone, and azithromycin, Dr. David Altarac, chief medical officer at Innoviva Specialty Therapeutics, said in an email.
“Rising resistance has steadily eroded the effectiveness of existing therapies, leaving clinicians with very limited options,” he said. “A novel, oral agent like zoliflodacin has the potential to meaningfully strengthen our treatment arsenal, support antimicrobial-resistance stewardship, and help slow the spread of a disease that remains a major public-health concern worldwide.”
Zoliflodacin also was developed solely for the treatment of gonorrhea, Balasegaram said, which limits its use for other types of bacterial infections.
That limited use reduces the risk of the medication being overly prescribed for other type of infections, thus leading to bacteria becoming so familiar with it that they may develop a resistance to it.
“We’ve made that part of the strategy from the outset,” Balasegaram said.
“Bacteria are smart. They can pass resistant mechanisms between each other,” he said. “What is very exciting is that there are these two new treatments coming out for this disease, where we haven’t had any new treatments coming out for a long time, where we’re now seeing 80 million-plus new infections globally each year, and where we’re seeing the emergence of drug resistance. So, this is really timely.”
Balasegaram worked on a large trial, the results of which were published Thursday in the journal The Lancet, that found that a single oral dose of zoliflodacin worked about as well as the current standard treatment: a ceftriaxone injection paired with an oral dose of the antibiotic azithromycin. Both approaches also showed similar safety results.
The study included more than 900 gonorrhea patients, ages 12 and older, treated at clinics in Belgium, the Netherlands, South Africa, Thailand and the United States.
After treatment, about 90.9% of those patients given zoliflodacin were cured, compared with about 96.2% of those who received the standard treatment.
Side effects in both groups were mostly mild or moderate, and no serious adverse events were reported. The researchers found that the most common treatment-related adverse events in the zoliflodacin group were headache or certain changes in white blood cell counts. For those who received the standard treatment, the most common were pain at the injection site, diarrhea and similar white blood cell changes.
“Taken together, the data suggest that zoliflodacin offers efficacy comparable to existing treatments, with a favorable and predictable safety profile, and the added potential benefit of a single-dose, oral regimen that may broaden access and ease of use,” Altarac said.
The cost of the medication has not yet been announced.
“We are committed to making our critically important drugs accessible and affordable for patients globally, including underserved markets. While we will share more details on pricing at a later date, we believe this medicine offers meaningful value for patients, healthcare providers, and health systems alike,” Pavel Raifeld, Innoviva’s CEO, said in an email Friday.
Separate research, published in April in The Lancet, found that gepotidacin also worked about as well as the current standard treatment, with no new safety concerns.
The trial, conducted between 2019 and 2023, included more than 600 people ages 12 and older who were diagnosed with gonorrhea in the urogenital area across six countries: Australia, Germany, Mexico, Spain, the United Kingdom and the United States.
About half of the participants were given two oral doses of gepotidacin about 10 to 12 hours apart. The others were given ceftriaxone and azithromycin.
After treatment, about 92.6% of those who were given gepotidacin were cured, compared with about 91.2% of those who got the current standard treatment.
The gepotidacin group had higher rates of adverse events and drug-related adverse events, mainly due to gastrointestinal issues, but almost all were mild or moderate. No severe or serious adverse events were reported.
The manufacturer’s list price of gepotidacin is $1,900 for a 20-tablet bottle, according to a GSK spokesperson. The full course of treatment for gonorrhea is eight tablets, and the list price does not reflect the final cost for patients, with or without insurance.
Although the development of new gonorrhea medications has been widely praised, some experts warn that efforts to fight the rise of drug-resistant gonorrhea must continue. For instance, there is some concern that strains of gonorrhea may eventually develop resistance to gepotidacin, according to a comment paper published in April in The Lancet.
Therefore, “preclinical and clinical development of additional gonorrhoea treatments remains important,” wrote Magnus Unemo of Örebro University in Sweden and Teodora Wi of the World Health Organization in Switzerland. “Gepotidacin is promising for the treatment of gonorrhoea, but the challenges to retain gonorrhoea as a treatable infection will continue.”





